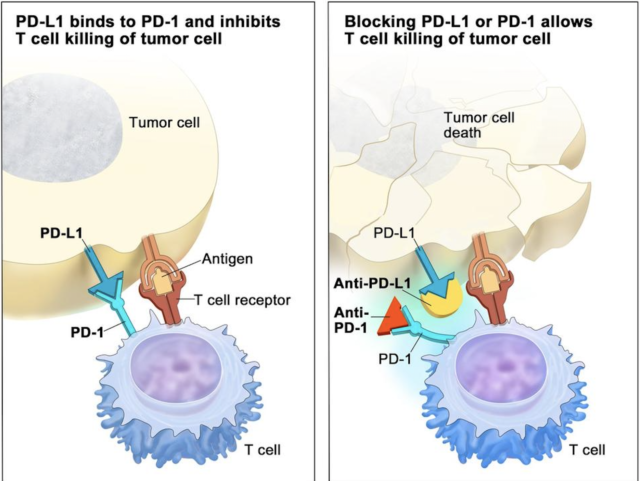
Keytruda (pembrolizumab) is an immune checkpoint inhibitor that gives patients with certain cancers another treatment option. Although, Keytruda has had successful outcomes, its use has created a roadblock, when trying to determine the response or reaction a tumor will or will not have to the therapy.
In New York City, at the Memorial Sloan Kettering Cancer Center, a more exact piece of the puzzle in immunotherapy has been unearthed. Found in Nature Genetics, the Kettering Cancer Center clinical study and research team identified cancerous cells that have an increased amount of DNA damage, were more likely to react better to immune checkpoint inhibitors (ICI), like Keytruda.
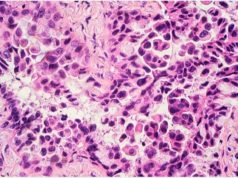
Tumor mutation burden (TMB), the focus in the study, is the numerical number of DNA or faults in the DNA that contains a tumor. According to a surgical oncologist, Dr. Luc Morris- a small number of studies that are centered around TMB have actually been completed, contrary to assumptions. With the assistance of an MSK-Impact assay-which is a tool that is used to target the generation sequencing of tumor tissue against other tissue specimens- the research team studied the DNA samples from 1,662 stage IV metastatic cancer patients that were treated with an immune checkpoint inhibitor and the DNA from 5,371 of the same untreated group type.
The results of the study showed that cancer genes with a high mutation number reacted 20% better with ICI treatment, than low mutation genes. However, these results were not comparable to tumors found in the brain or breast cancer tumors which are not routinely treated with ICI’s.
The successful outcome of the study was admittedly mysterious. However, the team did formulate a hypothesis that explains the reason for the connection: the more mutations found in a cell, the more likely that cell is to produce impaired proteins, called neoantigens. These neoantigens are increasingly abnormal and are identified as foreign to the body’s immune system. As a result, the immune system attacks them as they would a virus or bacteria.
The study completed by the Memorial Sloan Kettering Cancer Center of New York City, is the largest and most involved study of high tumor mutation burden, that has been successfully treated with immunotherapy. Although, other clinical trials have been completed on the same premise, certain studies under that umbrella targeted specific cancer types-including lung melanomas.
Yes- some trial participating patients did benefit from the study, while others did not; which shows health care professionals, clinicians and scientists still have more pieces to the puzzle to research. Dr. Morris, of MSKCC, is encouraged and optimistic that the data collected will lead to future studies of inclusive cancer types, to find a more universal treatment method.